초록접수 현황
| 20F-171 | 구연 발표 |
3-Dimensional Computed Tomographic Assessment Predicts Conduction Block and Paravalvular Leakage After Rapid-Deployment Aortic Valve Replacement
¹Sung Jun Park*, ¹Younju Rhee*, ²Chee-hoon Lee, ¹Ho Jin Kim, ¹Joon Bum Kim, ¹Suk Jung Choo, ¹Jae Won Lee
¹Department of Thoracic and Cardiovascular Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, South Korea
²Department of Thoracic and Cardiovascular Surgery, Pusan National University Yangsan Hospital, Medical Research Institute of Pusan National University, Busan, South Korea
Purpose : In the rapid deployment aortic valve (AV) replacement (RDAVR), complete atrio-ventricular block (CAVB) and paravalvular leakage (PVL) remain unresolved complications, and optimal valve-sizing may be important to minimize these complications. We sought to determine the impacts of prosthetic sizes relative to anatomic profiles of the AV on the occurrence of CAVB or PVL after RDAVR.
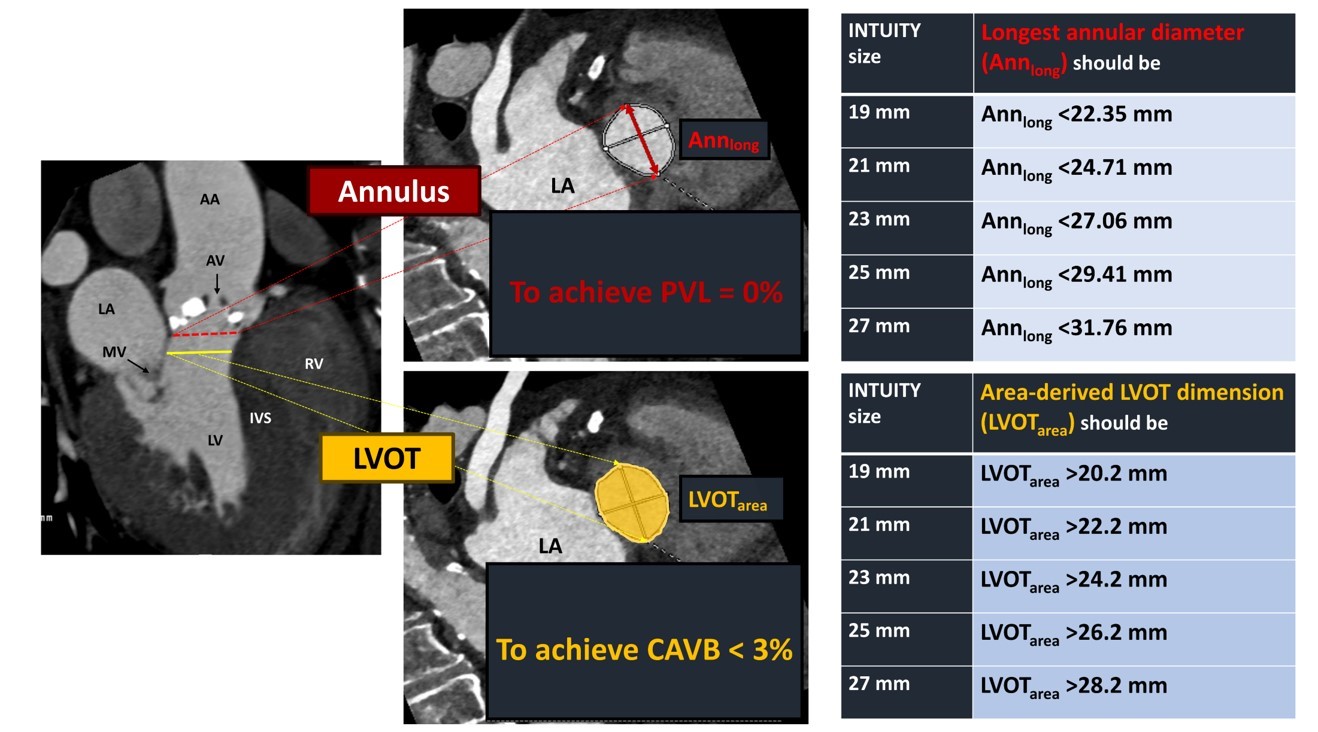
Methods : We analyzed 187 patients who had undergone preoperative multi-detector computed tomographic (CT) evaluation and RDAVR using INTUITY between Feb 2016 and Dec 2019. CAVB requiring permanent pacemaker implantation (PMI) and PVL (≥mild) were outcomes of interest. The relative size of implants as opposed to cross-sectional dimensions of recipients’ AV annulus and left ventricular outflow tract (LVOT) were calculated.
Results : CAVB was associated with oversizing of RDAVR (RDAVR frame-width minus average diameter of LVOT calculated from the cross-sectional area [ΔLVOTarea]: odds ratio [OR], 2.05; 95% confidence interval [CI], 1.28-3.30): This was with the area under the curve (AUC) of 0.78 (95% CI, 0.64-0.93). The projective probability of CAVB less than 3% was obtained when the ΔLVOTarea was <1.3. In contrast, PVL was associated with under-sized RDAVR (RDAVR size divided by longest diameter of AV annulus [Index Annlong]: OR, 0.64; 95% CI, 0.51-0.79): This was with AUC of 0.94 (95% CI, 0.90-0.98).
Conclusion : CT parameters derived from AV annulus and LVOT are highly reliable in the prediction of CAVB or PVL after RDAVR. Our data may justify CT-based sizing of prosthesis in RDAVR.
Methods : We analyzed 187 patients who had undergone preoperative multi-detector computed tomographic (CT) evaluation and RDAVR using INTUITY between Feb 2016 and Dec 2019. CAVB requiring permanent pacemaker implantation (PMI) and PVL (≥mild) were outcomes of interest. The relative size of implants as opposed to cross-sectional dimensions of recipients’ AV annulus and left ventricular outflow tract (LVOT) were calculated.
Results : CAVB was associated with oversizing of RDAVR (RDAVR frame-width minus average diameter of LVOT calculated from the cross-sectional area [ΔLVOTarea]: odds ratio [OR], 2.05; 95% confidence interval [CI], 1.28-3.30): This was with the area under the curve (AUC) of 0.78 (95% CI, 0.64-0.93). The projective probability of CAVB less than 3% was obtained when the ΔLVOTarea was <1.3. In contrast, PVL was associated with under-sized RDAVR (RDAVR size divided by longest diameter of AV annulus [Index Annlong]: OR, 0.64; 95% CI, 0.51-0.79): This was with AUC of 0.94 (95% CI, 0.90-0.98).
Conclusion : CT parameters derived from AV annulus and LVOT are highly reliable in the prediction of CAVB or PVL after RDAVR. Our data may justify CT-based sizing of prosthesis in RDAVR.
책임저자: Jae Won Lee
Department of Thoracic and Cardiovascular Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, South Korea
발표자: Jae Won Lee, E-mail : jwlee@amc.seoul.kr


