초록접수 현황
| 19F-254 | 구연 발표 |
Risk Factors and Treatment Outcome of Post-Pneumonectomy Bronchopleural Fistula (BPF)
Soo Hwan Choi¹, Yong Jin Chang¹, Jong Hee Seo², Young Jo Sa³, Jung Suk Choi⁴, Jae Shin Yoon⁴, Seok Whan Moon⁴, Jae Kil Park⁴, Deog gon Cho¹
¹Department of Thoracic and Cardiovascular Surgery, St. Vincent`s Hospital, The Catholic University College of Medicine, Gyeonggi-do, Republic of Korea, ²Department of Thoracic and Cardiovascular Surgery, Incheon St. Mary`s Hospital, The Catholic University College of Medicine, Incheon, Republic of Korea, ³Department of Thoracic and Cardiovascular Surgery, Yeouido St. Mary’s Hospital, The Catholic University College of Medicine, Seoul, Republic of Korea, ⁴Department of Thoracic and Cardiovascular Surgery, Seoul St. Mary’s Hospital, The Catholic University College of Medicine, Seoul, Republic of Korea
Purpose : The most radical procedure in thoracic surgery, pneumonectomy is considered by some to be a disease, procedure itself. Though, improvement in patient optimization, surgical technique, and multidisciplinary care, still a high morbidity rate (about 50%) is reported. Bronchopleural Fistula (BPF) is the most fatal complication after pneumonectomy and mortality rate is up to 71%. Prevention is paramount and treatment is troublesome. But, risk factors are controversial and rescue treatment is not definite. Here, we report our surgical experience of pneumonectomy in various disease and treatment outcome of BPF.
Methods : From February 2003 to February 2019, we retrospectively reviewed the medical records in four hospitals.
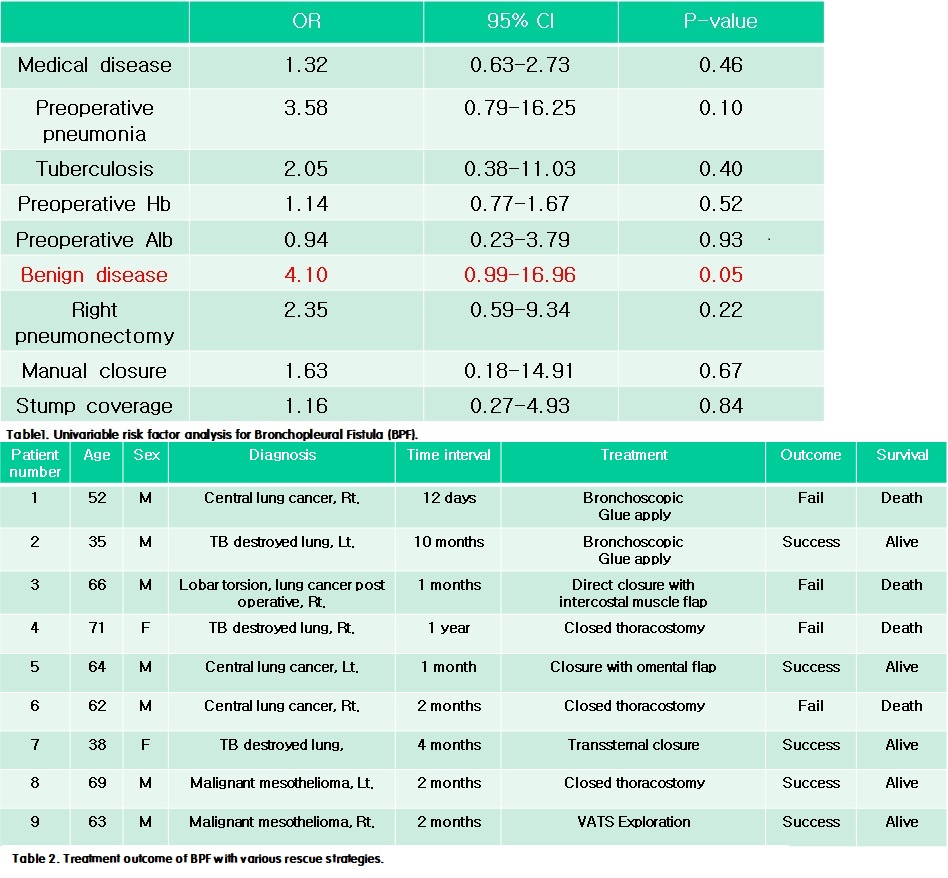
Results : Total one hundred and twenty-four patients were enrolled. The mean age was 60.1±11.5 years old. Male and female patients were 100 (80.6%) and 24 (19.4%). Pneumonectomy was applied in malignant disease (n=101, 81.2%), benign disease (n=20, 16.1%), and post lung resection complications (n=3, 2.4%). BPF occurrence rate was 7.3% and pneumonectomy mortality rate was 4.8%. In comparison between BPF group and no-BPF group, pneumonectomy for benign disease was more frequently performed in BPF group (33.3%) than no-BPF group (15.6%, p-value 0.02). Risk factor analysis and treatment outcomes are shown table 1 and 2.
Conclusion : In our study, pneumonectomy for benign disease, especially infectious disease is the only possible risk factor. Various types of treatment are applied to treat of control BPF, the principles are infection control, drainage, and space obliteration.
Methods : From February 2003 to February 2019, we retrospectively reviewed the medical records in four hospitals.
Results : Total one hundred and twenty-four patients were enrolled. The mean age was 60.1±11.5 years old. Male and female patients were 100 (80.6%) and 24 (19.4%). Pneumonectomy was applied in malignant disease (n=101, 81.2%), benign disease (n=20, 16.1%), and post lung resection complications (n=3, 2.4%). BPF occurrence rate was 7.3% and pneumonectomy mortality rate was 4.8%. In comparison between BPF group and no-BPF group, pneumonectomy for benign disease was more frequently performed in BPF group (33.3%) than no-BPF group (15.6%, p-value 0.02). Risk factor analysis and treatment outcomes are shown table 1 and 2.
Conclusion : In our study, pneumonectomy for benign disease, especially infectious disease is the only possible risk factor. Various types of treatment are applied to treat of control BPF, the principles are infection control, drainage, and space obliteration.
책임저자: Deog Gon Cho
Department of Thoracic and Cardiovascular Surgery, St. Vincent`s Hospital, The Catholic University College of Medicine, Gyeonggi-do, Republic of Korea
발표자: Jung Suk Choi, E-mail : macommy@naver.com