초록접수 현황
| 19F-238 | 구연 미채택시 포럼 발표 |
Pathologic Tumor Response after Neoadjuvant Concurrent Chemoradiotherapy in Stage IIIA(N2) Non-small Cell Lung Cancer: Implication of major Pathologic Response and Residual Tumor Cells on the Systemic Failure
Junghee Lee¹, Hyunjin Kim², Yong Soo Choi¹, Joungho Han², Sumin Shin¹, Jong Ho Cho¹, Hong Kwan Kim¹, Jhingook Kim¹, Jae Ill Zo¹, Young Mog Shim¹
¹Department of Thoracic and Cardiovascular Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea, ²Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea
Purpose : This study aimed to investigate whether major pathologic response (MPR, ≤ 10% of residual tumor cells) predicts survival and systemic metastasis after surgical resection following neoadjuvant chemoradiation in patients with stage IIIA (N2) lung cancer.
Methods : An institutional database between 2007 and 2016 was reviewed retrospectively. Eligible 479 patients had pathological stage IIIA(N2) lung cancer with histologically confirmed clinical N2. Trimodal therapy mainly comprised of neoadjuvant chemoradiotherapy with two cycles of paclitaxel /cisplatin and 44 Gy radiation, thereafter surgical resection and adjuvant therapy. Optimal cut-off percentage of viable tumor was estimated for systemic recurrence and overall survival.
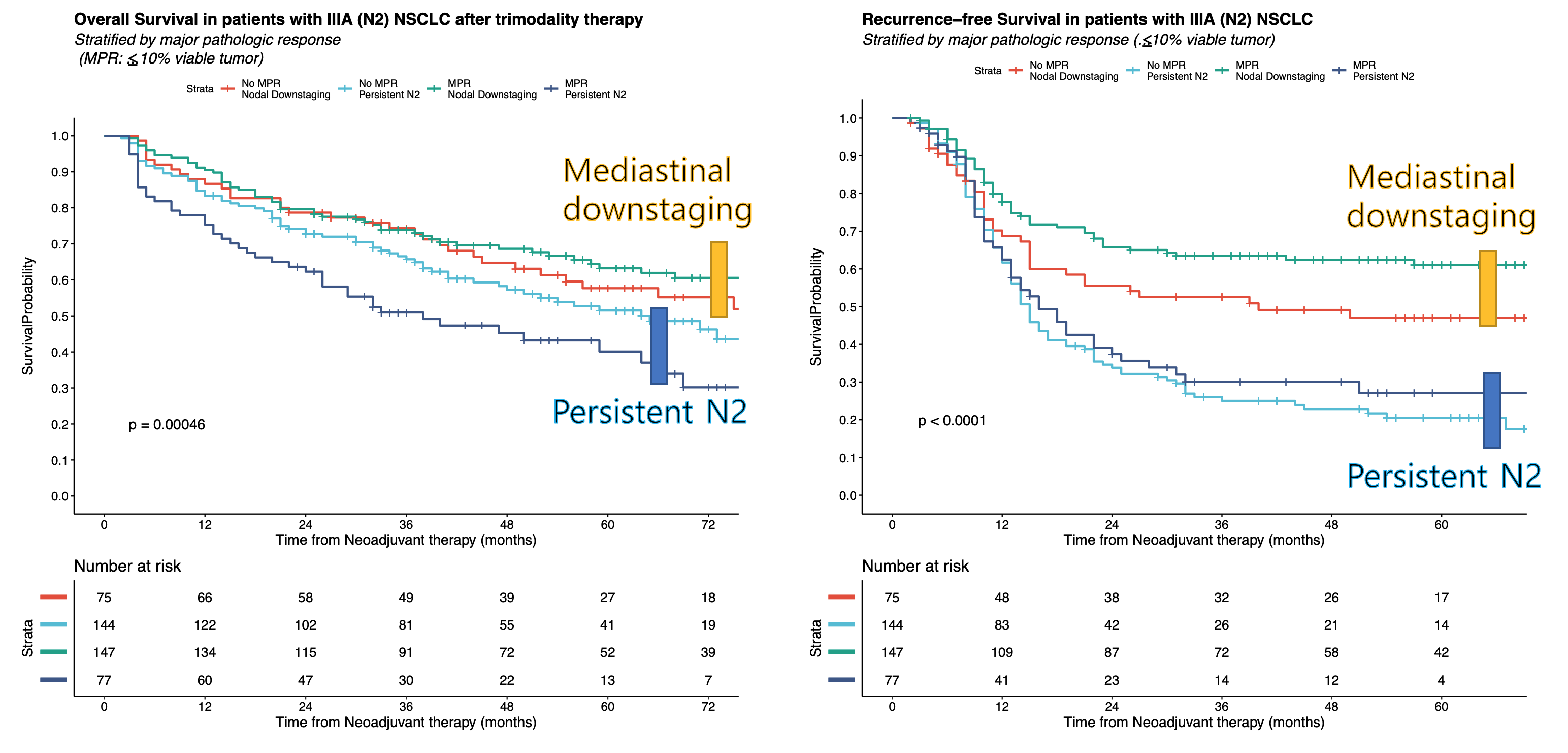
Results : Study population consisted of persistent N2 (ypN2, n=235) and mediastinal downstaging (ypN0-1, n=244). Mediastinal downstaging group had better tumor response (median % of viable tumor) to neoadjuvant chemoradiotherapy; 40% in ypN2 versus 5% in ypN0-1 (p<0.001). MPR was also higher in ypN0-1 (66.2%) than ypN2 (34.8%) (p<0.001). MPR was predictive of recurrence-free and overall survival in ypN2, but not in ypN0-1. The optimal cutoff percentage of viable tumor for systemic recurrence-free survival was 25% in ypN2 (p=0.031) and 1% in ypN0-1 (p=0.0052). On multivariate analysis, histologic subtype of squamous carcinoma was a favorable factor for systemic recurrence-free survival (HR 0.33; p<0.001 in ypN0-1, HR 0.53; p <0.001 in ypN2).
Conclusion : Major pathologic response was a good prognostic factor in persistent N2 after neoadjuvant chemoradiation followed by surgery and adjuvant therapy for stage IIIA(N2) lung cancer.
Methods : An institutional database between 2007 and 2016 was reviewed retrospectively. Eligible 479 patients had pathological stage IIIA(N2) lung cancer with histologically confirmed clinical N2. Trimodal therapy mainly comprised of neoadjuvant chemoradiotherapy with two cycles of paclitaxel /cisplatin and 44 Gy radiation, thereafter surgical resection and adjuvant therapy. Optimal cut-off percentage of viable tumor was estimated for systemic recurrence and overall survival.
Results : Study population consisted of persistent N2 (ypN2, n=235) and mediastinal downstaging (ypN0-1, n=244). Mediastinal downstaging group had better tumor response (median % of viable tumor) to neoadjuvant chemoradiotherapy; 40% in ypN2 versus 5% in ypN0-1 (p<0.001). MPR was also higher in ypN0-1 (66.2%) than ypN2 (34.8%) (p<0.001). MPR was predictive of recurrence-free and overall survival in ypN2, but not in ypN0-1. The optimal cutoff percentage of viable tumor for systemic recurrence-free survival was 25% in ypN2 (p=0.031) and 1% in ypN0-1 (p=0.0052). On multivariate analysis, histologic subtype of squamous carcinoma was a favorable factor for systemic recurrence-free survival (HR 0.33; p<0.001 in ypN0-1, HR 0.53; p <0.001 in ypN2).
Conclusion : Major pathologic response was a good prognostic factor in persistent N2 after neoadjuvant chemoradiation followed by surgery and adjuvant therapy for stage IIIA(N2) lung cancer.
책임저자: Yong Soo Choi
Department of Thoracic and Cardiovascular Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea
발표자: Junghee Lee, E-mail : ts.junghee@gmail.com