초록접수 현황
| 19F-209 | 구연 발표 |
Successful VATS Lobectomy and Complete Mediastinal Lymph Node Dissection for Clinical N2 Lung Cancer after Neoadjuvant Concurrent Chemoradiation Therapy: Comparison of Operative Outcomes between Early-period and Late-period.
Byung Jo Park¹, Yong Soo Choi¹, Yeong Jeong Jeon¹, Kyungjong Lee², Hongryull Pyo³, Jin Seok Ahn⁴
¹Department of Thoracic and Cardiovascular Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea, ²Division of Pulmonary and Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea, Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea, ⁴Division of Hematology-Oncology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea
Purpose : We have applied 3D-thoracoscope, energy-device instead of 2D-thoracoscope, monopolar electrocautery hook for VATS lobectomy since July 2016. The aim of this study is to compare the operative outcomes of VATS lobectomy following neoadjuvant CCRT in clinical N2 lung cancer before vs. after the use of 3D-thoracoscope and energy device.
Methods : VATS lobectomy and mediastinal lymph node dissection following neoadjuvant CCRT was attempted in 79 patients with clinical N2 lung cancer from Jan 2009 to May 2019. Except for the learning-period, 52 patients who underwent surgery were enrolled. The study period was divided into early-period (23 patients, June 2012 to June 2016) and late-period (29 patients, July 2016 to May 2019). We conducted intention-to-treat analysis and per-protocol analysis.
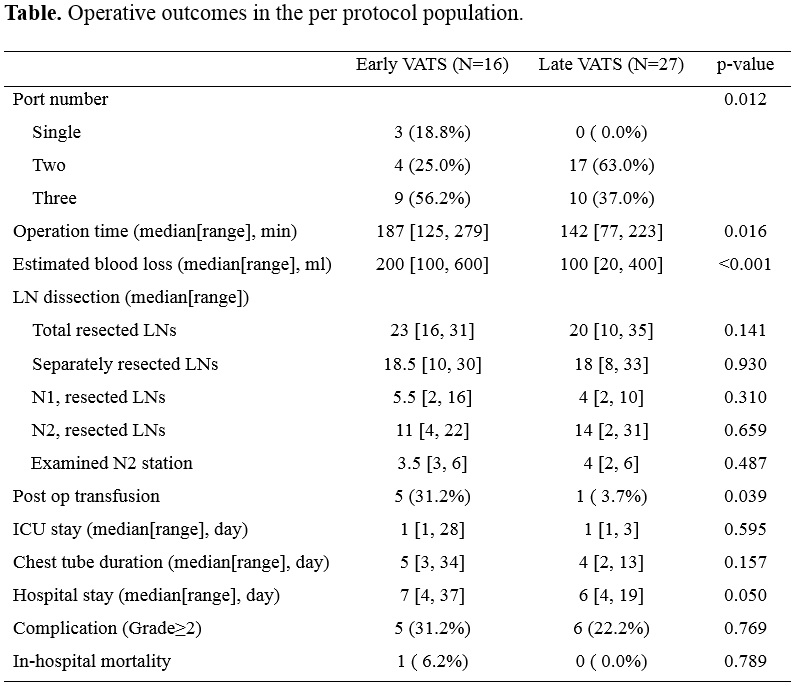
Results : In the early-period, 16 patients (69.6%) had completed VATS lobectomy and 27 patients (93.1%) in the late-period (p=0.063). On the per-protocol analysis, the operation time (median 142min vs. 187min, p=0.016), operative blood loss (median 100ml vs. 200ml, p<0.001), and hospital stay after surgery (median 6 vs. 7 days, p=0.050) were reduced in the late-period compared to the early-period. There was no significant difference in operative complication (Clavien-Dindo classification Gr≥2, 24.1% vs. 39.1%, p=0.389), the number of total resected lymph nodes (median 20 vs. 23, p=0.141) or resected N2 nodes (median 14 vs. 11, p=0.659).
Conclusion : Application of 3D-thoracoscope, energy-device and probably accumulation of experience have improved surgical outcomes such as operation time, blood loss, and hospital stay in VATS lobectomy for clinical N2 lung cancer following neoadjuvant CCRT.
Methods : VATS lobectomy and mediastinal lymph node dissection following neoadjuvant CCRT was attempted in 79 patients with clinical N2 lung cancer from Jan 2009 to May 2019. Except for the learning-period, 52 patients who underwent surgery were enrolled. The study period was divided into early-period (23 patients, June 2012 to June 2016) and late-period (29 patients, July 2016 to May 2019). We conducted intention-to-treat analysis and per-protocol analysis.
Results : In the early-period, 16 patients (69.6%) had completed VATS lobectomy and 27 patients (93.1%) in the late-period (p=0.063). On the per-protocol analysis, the operation time (median 142min vs. 187min, p=0.016), operative blood loss (median 100ml vs. 200ml, p<0.001), and hospital stay after surgery (median 6 vs. 7 days, p=0.050) were reduced in the late-period compared to the early-period. There was no significant difference in operative complication (Clavien-Dindo classification Gr≥2, 24.1% vs. 39.1%, p=0.389), the number of total resected lymph nodes (median 20 vs. 23, p=0.141) or resected N2 nodes (median 14 vs. 11, p=0.659).
Conclusion : Application of 3D-thoracoscope, energy-device and probably accumulation of experience have improved surgical outcomes such as operation time, blood loss, and hospital stay in VATS lobectomy for clinical N2 lung cancer following neoadjuvant CCRT.
책임저자: Yong Soo Choi
Department of Thoracic and Cardiovascular Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea
발표자: Byung Jo Park, E-mail : skddls05@naver.com