초록접수 현황
| 19F-056 | 구연 미채택시 포럼 발표 |
The Efficacy of Intranasal Mupirocin Prophylaxis in Aortic Surgery: Randomized Controlled Trial
Myeong Su Kim¹, Suk-Won Song², Tae-Hoon Kim², Ha Lee², Woon Heo³, Kyung-Jong Yoo⁴, Byung Chul Chang⁵, Bum-Koo Cho⁶
¹Department of Throracic and Cardiovascular Surgery, Armed Forces Capital Hospital, Gyeonggi-do, Republic of Korea, ²Department of Thoracic and Cardiovascular Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea, ³Department of Thoracic and Cardiovascular Surgery, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan Republic of Korea, ⁴Department of Thoracic and Cardiovascular Surgery, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea, ⁵Department of Thoracic and Cardiovascular Surgery, CHA Bundang Medical Center, CHA University College of Medicine, Gyeonggi-do, Republic of Korea, ⁶The Korea Heart Foundation, Seoul, Republic of Korea
Purpose : The aim of this study was to determine the efficacy of intranasal mupirocin prophylaxis for preventing perioperative Methicillin-resistant Staphylococcus aureus (MRSA) infections in patients undergoing thoracic or abdominal aortic surgery.
Methods : A prospective, randomized controlled trial was conducted between 2017 and 2018. The patients (n=145) who underwent open aortic repair were enrolled. Seventy-two patients were patients with intranasal mupirocin prophylaxis (group M) and the others were without prophylactic intervention (group C, n=73).
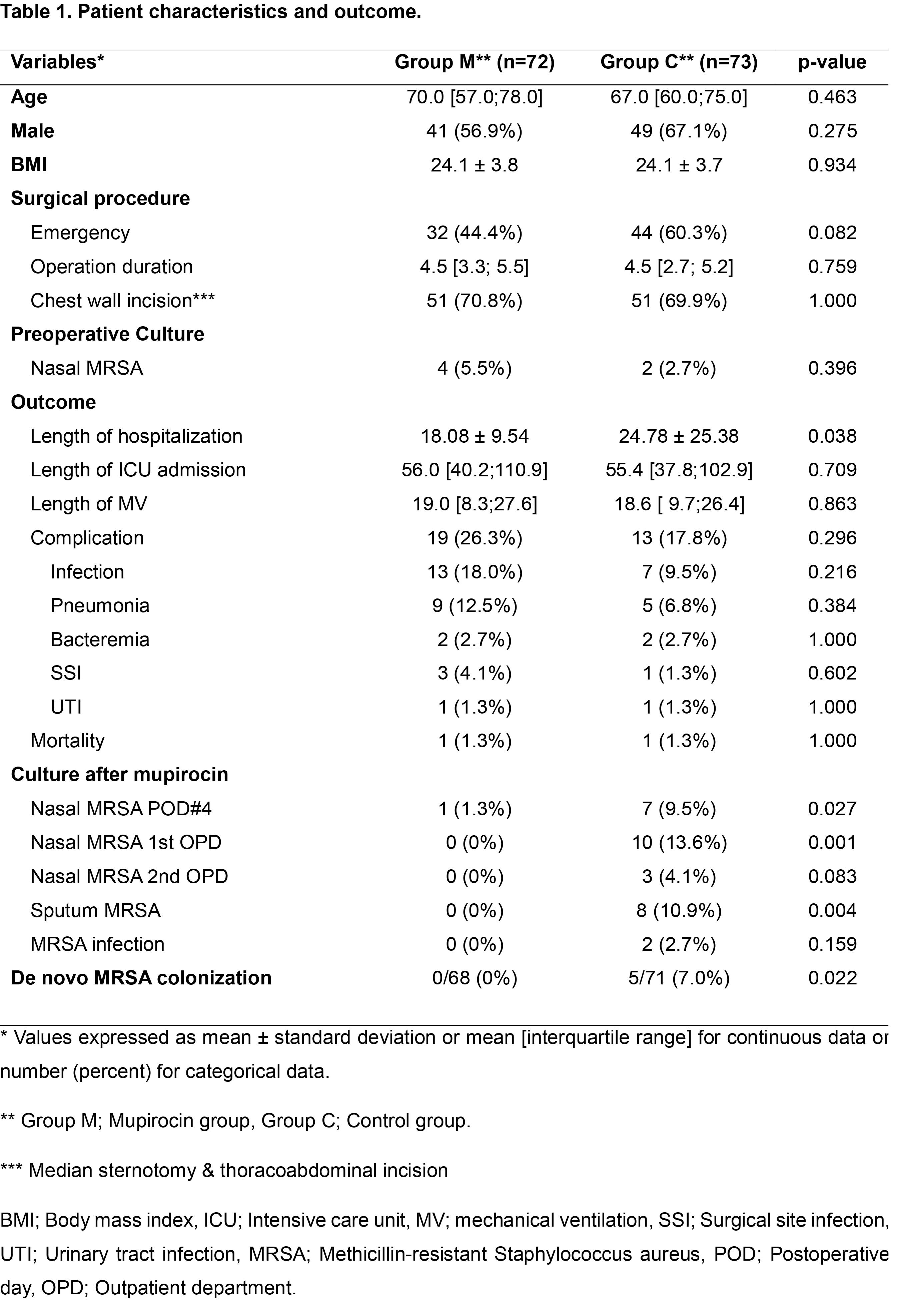
Results : There was no significant intranasal mupirocin prophylaxis-related complication. The incidence of surgical site infection and other infection-related complication was not significantly different between 2 groups (Table 1). In group M, length of hospitalization was shorter than group C (18.1 days vs. 24.8 days, p=0.038). Of entire cohort, 6 patients preoperatively carried MRSA in their nares and the proportion was not significantly different between two groups (group M, 5.5% vs. group C 2.7%, p=0.396). At the time of 4th day after operation and the first visit after discharge, the incidence of nasal MRSA (+) was significantly lower in group M compared to group C (1.3% vs. 9.5%, p=0.027; 0% vs. 13.6%, p=0.001, respectively). The incidence of sputum MRSA (+) was significantly lower in group M (0% vs. 10.9%, p=0.004). De novo MRSA colonization rate was significantly higher in group C (0% vs. 7.0%, p=0.022).
Conclusion : Intranasal mupirocin prophylaxis was safe and easy to apply. Furthermore, it seemed to be beneficial for decreasing length of hospitalization and de novo MRSA colonization rate in nares and sputum.
Methods : A prospective, randomized controlled trial was conducted between 2017 and 2018. The patients (n=145) who underwent open aortic repair were enrolled. Seventy-two patients were patients with intranasal mupirocin prophylaxis (group M) and the others were without prophylactic intervention (group C, n=73).
Results : There was no significant intranasal mupirocin prophylaxis-related complication. The incidence of surgical site infection and other infection-related complication was not significantly different between 2 groups (Table 1). In group M, length of hospitalization was shorter than group C (18.1 days vs. 24.8 days, p=0.038). Of entire cohort, 6 patients preoperatively carried MRSA in their nares and the proportion was not significantly different between two groups (group M, 5.5% vs. group C 2.7%, p=0.396). At the time of 4th day after operation and the first visit after discharge, the incidence of nasal MRSA (+) was significantly lower in group M compared to group C (1.3% vs. 9.5%, p=0.027; 0% vs. 13.6%, p=0.001, respectively). The incidence of sputum MRSA (+) was significantly lower in group M (0% vs. 10.9%, p=0.004). De novo MRSA colonization rate was significantly higher in group C (0% vs. 7.0%, p=0.022).
Conclusion : Intranasal mupirocin prophylaxis was safe and easy to apply. Furthermore, it seemed to be beneficial for decreasing length of hospitalization and de novo MRSA colonization rate in nares and sputum.
책임저자: Suk-Won Song
Department of Thoracic and Cardiovascular Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea
발표자: Myeong Su Kim, E-mail : mmotion11@gmail.com