초록접수 현황
| 16F-247 | 구연 발표 |
Comparision of Oncologic Outcomes for Pathologic N1/N2 Non-small Cell Lung Cancer by Thoracoscopic Surgery Versus Thoracotomy: A Propensity Score Matching Study
Yoohwa Hwang, Kwanyong Hyun, Samina Park, Hyun Joo Lee, In-Kyu Park, Young Tae Kim, Chang Hyun Kang
Department of Thoracic and Cardiovascular Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
Background : The safety and feasibility of systemic mediastinal LN dissection by thoracoscopic lobectomy remain controversial, especially concerning the problem whether conversion from VATS to thoracotomy in necessary in postoperatively lymph node metastasis. The aim of this study was to compare oncologic outcomes including overall and disease free survival between thoracoscopic and thoracotomy lobectomy for the patients with pathologic N1/N2 NSCLC.
Methods : We conducted a retrospective review of 590 patients who had a complete resection with systemic lymph node dissection for pathologic N1/N2 NSCLC at out institute from Jan 2006 to December 2013. The patients were divided into a thoracoscopic group(Group V, n=161) and thoracotomy group(Group T, n=429). Preoperative clinical parameter including gender, age, smoking history, comorbidity, FEV1, tumor size, histology, clinical TNM stage, pathologic N stage, operative extent were used for propensity score matching. After propensity score matching, 120 thoracoscopy and thoracotomy group were selected and compared
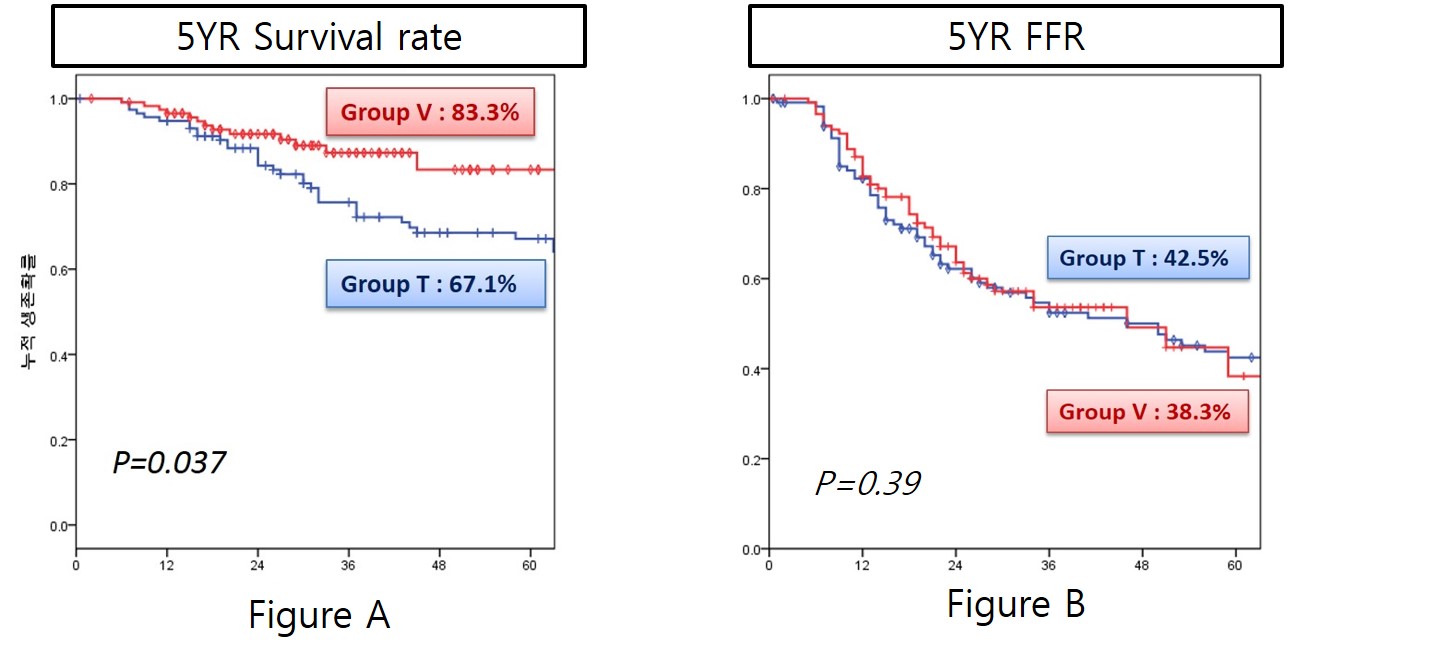
Results : There were no difference in clinical and pathologic TNM stage between two groups. Although operative mortality and postoperative complications were not significantly different between two groups, operation time and hospital stay was significantly shorter (166.6±57.4min vs 203.8±75.5min, p<0.001, 7days vs 10days, p=0.004) and postoperative pulmonary complication rate were significantly lower in Group V.(p=0.03). Total number of LN was 31.2±10.6 in groupT vs 27.2±10.5 in groupV.(p=0.004) The rate of nodal metastasis (number of metastatic nodes/number of dissected nodes) was similar between the two groups.(p=0.78) Median follow-up was 72months. Both the incidence and distribution of recurrence were similar. (5yr FFR 42.5%vs38.3%, p=0.83, Figure A) The 5-year overall survival was significantly higher in the thoracoscopic groups. (83.3%vs67.1%, p=0.037, Figure B)
Conclusion : Thoracoscopic lobectomy could be an acceptable and valuable approach in selected pathologic N1 or N2 NSCLC, providing the safety and feasibility of systemic mediastinal LN dissection despite the presence of lymph node metastasis and lower postopertive complication rate.
Methods : We conducted a retrospective review of 590 patients who had a complete resection with systemic lymph node dissection for pathologic N1/N2 NSCLC at out institute from Jan 2006 to December 2013. The patients were divided into a thoracoscopic group(Group V, n=161) and thoracotomy group(Group T, n=429). Preoperative clinical parameter including gender, age, smoking history, comorbidity, FEV1, tumor size, histology, clinical TNM stage, pathologic N stage, operative extent were used for propensity score matching. After propensity score matching, 120 thoracoscopy and thoracotomy group were selected and compared
Results : There were no difference in clinical and pathologic TNM stage between two groups. Although operative mortality and postoperative complications were not significantly different between two groups, operation time and hospital stay was significantly shorter (166.6±57.4min vs 203.8±75.5min, p<0.001, 7days vs 10days, p=0.004) and postoperative pulmonary complication rate were significantly lower in Group V.(p=0.03). Total number of LN was 31.2±10.6 in groupT vs 27.2±10.5 in groupV.(p=0.004) The rate of nodal metastasis (number of metastatic nodes/number of dissected nodes) was similar between the two groups.(p=0.78) Median follow-up was 72months. Both the incidence and distribution of recurrence were similar. (5yr FFR 42.5%vs38.3%, p=0.83, Figure A) The 5-year overall survival was significantly higher in the thoracoscopic groups. (83.3%vs67.1%, p=0.037, Figure B)
Conclusion : Thoracoscopic lobectomy could be an acceptable and valuable approach in selected pathologic N1 or N2 NSCLC, providing the safety and feasibility of systemic mediastinal LN dissection despite the presence of lymph node metastasis and lower postopertive complication rate.
책임저자: Chang Hyun Kang
Department of Thoracic and Cardiovascular Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
발표자: Yoohwa Hwang, E-mail : yooflower@naver.com