초록접수 현황
| 16F-184 | 구연 발표 |
Impact of Lymph node Dissection in Surgery for Thymic Malignancies: Multi-institutional-propensity Matched Analysis
강창현¹, 황유화¹, 현관용¹, 박샘이나¹, 김응래¹, 이현주¹, 박인규¹, 김영태¹, 남경식², 변고은², 이창영², 이진구², 김대준², 정경영², 김석³, 이진희³, 조종호³, 최용수³, 김진국³, 조재일³, 심영목³, 복진산⁴, 황수경⁴, 이근동⁴, 최세훈⁴, 김형렬⁴, 김용희⁴, 김동관⁴, 박승일⁴
서울대학교 의과대학 서울대학교병원 흉부외과교실¹, 연세대학교 의과대학 세브란스병원 흉부외과학교실², 성균관대학교 의과대학 삼성서울병원 흉부외과학교실³, 울산대학교 의과대학 서울아산병원 흉부외과학교실⁴
Background : Surgical resection is the best treatment in thymic malignancy; however, the prognostic significance of nodal metastases is unclear and guidelines regarding lymph node dissection have not been suggested. The aim of this study is to analyze the prognostic implications of nodal metastases and role of lymph node dissection (LND) in thymic malignancy.
Methods : Between January 2000 and December 2013, 1,597 patients who underwent thymectomy due to thymic malignancy from multi-center database were retrospectively analyzed. Intentional LND was performed in 443 patients (27.7%). The patients were divided into LND+ and LND- group in thymoma and thymic carcinoma. Preoperative clinical parameter including age, gender, comorbidity, symptom, myasthenia gravis, performance status, tumor size, clinical Masaoka-Koaga stage, and lymphadenopathy in preoperative staging were used for propensity score matching. After propensity score matching, LND+ and LND- groups were matched in 580 patients in thymoma and 200 patients in thymic carcinoma, respectively.
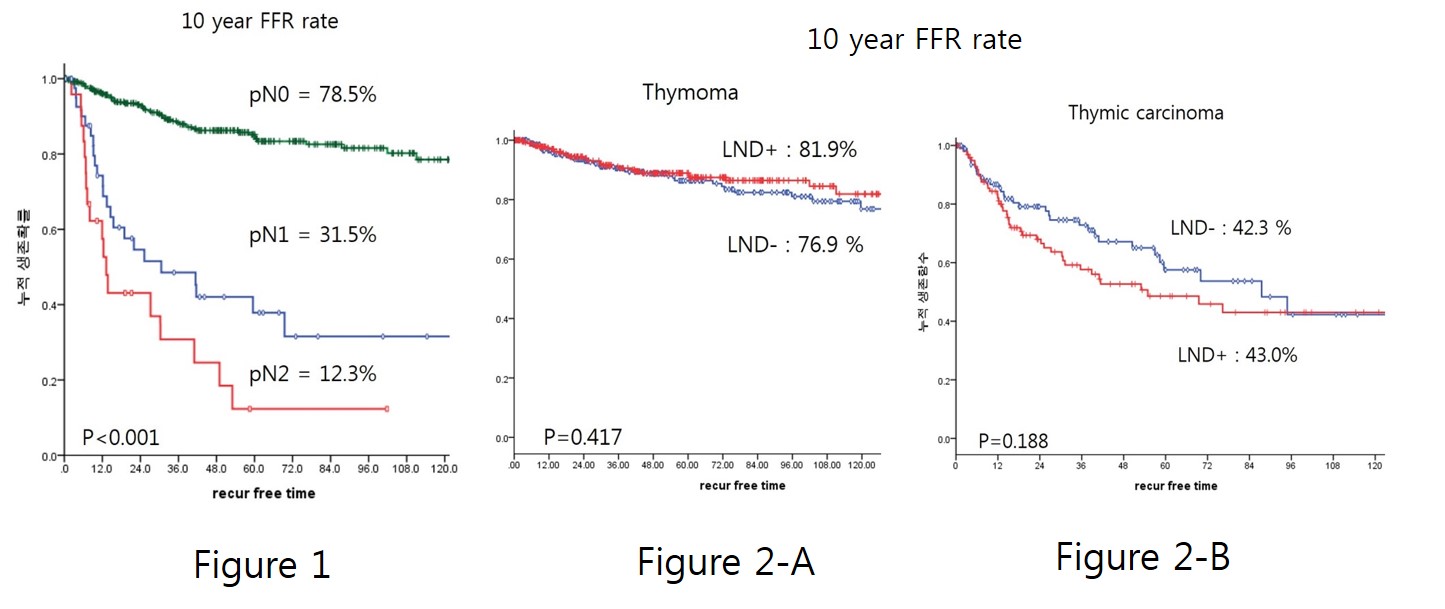
Results : Lymph Node metastasis was identified in 13 patients with thymoma (6.7%) and 47 patients with thymic carcinoma (32.7%). In multivariable analysis, thymic carcinoma (HR 19.2, p<0.001), the subtype of thymoma (A/AB/B1vsB2/B3, HR 4.6, p=0.02), and tumor size (HR 1.1, p=0.02) were significant predictive factors for nodal metastasis. In 10-year freedom from recurrence (FFR) rate, the pN1 and pN2 was significantly worse than that of the pN0 (p<0.001, Figure1). Intentional LN dissection did not increase operative mortality or complication in both of thymoma and thymic carcinoma group. There was no difference in 10-year FFR rate between LND+ and LND- groups (81.9% vs. 76.9%, p=0.42 in thymoma; 43.0% vs. 42.3%, p=0.19 in thymic carcinoma, Figure2).
Conclusion : Nodal status was an important prognostic factor in patients with thymic malignancies. Although LND did not improve long-term outcomes in thymic malignancies, LND can help identify pathologic stage more accurately.
Methods : Between January 2000 and December 2013, 1,597 patients who underwent thymectomy due to thymic malignancy from multi-center database were retrospectively analyzed. Intentional LND was performed in 443 patients (27.7%). The patients were divided into LND+ and LND- group in thymoma and thymic carcinoma. Preoperative clinical parameter including age, gender, comorbidity, symptom, myasthenia gravis, performance status, tumor size, clinical Masaoka-Koaga stage, and lymphadenopathy in preoperative staging were used for propensity score matching. After propensity score matching, LND+ and LND- groups were matched in 580 patients in thymoma and 200 patients in thymic carcinoma, respectively.
Results : Lymph Node metastasis was identified in 13 patients with thymoma (6.7%) and 47 patients with thymic carcinoma (32.7%). In multivariable analysis, thymic carcinoma (HR 19.2, p<0.001), the subtype of thymoma (A/AB/B1vsB2/B3, HR 4.6, p=0.02), and tumor size (HR 1.1, p=0.02) were significant predictive factors for nodal metastasis. In 10-year freedom from recurrence (FFR) rate, the pN1 and pN2 was significantly worse than that of the pN0 (p<0.001, Figure1). Intentional LN dissection did not increase operative mortality or complication in both of thymoma and thymic carcinoma group. There was no difference in 10-year FFR rate between LND+ and LND- groups (81.9% vs. 76.9%, p=0.42 in thymoma; 43.0% vs. 42.3%, p=0.19 in thymic carcinoma, Figure2).
Conclusion : Nodal status was an important prognostic factor in patients with thymic malignancies. Although LND did not improve long-term outcomes in thymic malignancies, LND can help identify pathologic stage more accurately.
책임저자: 강창현
서울대학교 의과대학 서울대학교병원 흉부외과교실
발표자: 강창현, E-mail : chkang@snu.ac.kr