초록접수 현황
| 16F-022 | 구연 발표 |
The Differential Roles of Lymphadenectomy in Surgical Treatment of Patients with Esophageal Cancer Based on Disease Stage and Neoadjuvant Treatment
Samina Park, MD, Kwanyong Hyun, MD, Yoohwa Hwang, MD, Hyun Joo Lee, MD, PhD, In Kyu Park, MD, PhD, Young Tae Kim, MD, PhD, Chang Hyun Kang, MD, PhD
Department of Thoracic and Cardiovascular Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
Background : The adequeate extent of lymphadenectomy is a controverial issue. This study aimed to elucidate the role of lymphadenectomy during surgical treatment of patients with esophageal cancer based on variable disease stage and neoadjuvant treatment.
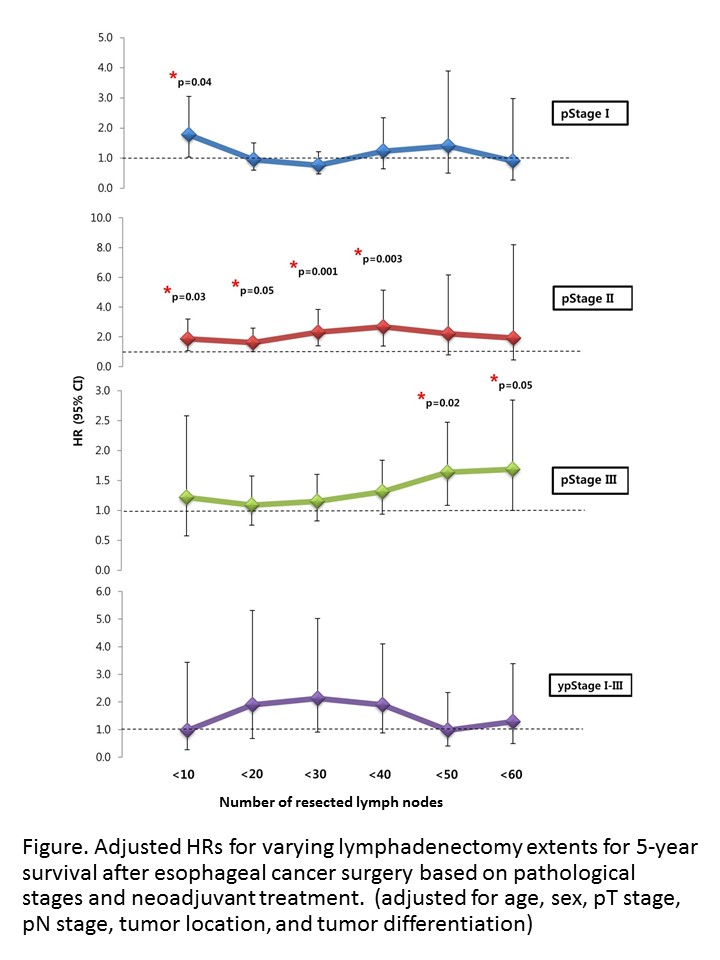
Methods : We reviewed medical records of patients who underwent esophagectomies for esophageal cancer between December 1994 and December 2015. A total of 840 patients were included in this study and divided into four groups according to pathological stages and neoadjuvant treatment. The effects of lymphadenectomy extent were measured using hazard ratios (HRs), which were analyzed according to the numbers of dissected lymph nodes in intervals of 10. HRs were adjusted for age, sex, pathologic T-stages, pathologic N-stages, tumor locations, and degrees of tumor differentiation.
Results : The median age was 64 years. Squamous cell carcinoma was diagnosed in 794 patients (94.5%), and 789 patients (93.9%) were male. The number of resected lymph nodes was significantly associated with survival of stage II (p=0.002, HR=0.975) and stage III (p=0.021, HR=0.991), whereas it was not associated with survival of stage I (p=0.554, HR=0.995) or those who received neoadjuvant treatment (p=0.392, HR=0.993). Serial comparison of HRs demonstated that the effect of lymphadectectomy extent on survival differed depending on stage. For stage I disease, dissection of more than 20 lymph nodes was not associated with prolonged patient survival. For stage II disease, patient survival improved continously after lymphadenectomies of up to 40 nodes, and there was no further increase in survival thereafter. For stage III disease, a patient survival benefit was identifed when more than 50 lymph nodes were dissected. In the neoadjuvant treatment group, the lymphadenectomy extent did not influence patient survival.
Conclusion : Lymphadenectomy influenced patient survival differently depending on disease stage and neoadjuvant treatment. More extensive lymphadenectomies are necessary, especially when treating advanced disease, to improve long-term survival of patients with esophageal cancer.
Methods : We reviewed medical records of patients who underwent esophagectomies for esophageal cancer between December 1994 and December 2015. A total of 840 patients were included in this study and divided into four groups according to pathological stages and neoadjuvant treatment. The effects of lymphadenectomy extent were measured using hazard ratios (HRs), which were analyzed according to the numbers of dissected lymph nodes in intervals of 10. HRs were adjusted for age, sex, pathologic T-stages, pathologic N-stages, tumor locations, and degrees of tumor differentiation.
Results : The median age was 64 years. Squamous cell carcinoma was diagnosed in 794 patients (94.5%), and 789 patients (93.9%) were male. The number of resected lymph nodes was significantly associated with survival of stage II (p=0.002, HR=0.975) and stage III (p=0.021, HR=0.991), whereas it was not associated with survival of stage I (p=0.554, HR=0.995) or those who received neoadjuvant treatment (p=0.392, HR=0.993). Serial comparison of HRs demonstated that the effect of lymphadectectomy extent on survival differed depending on stage. For stage I disease, dissection of more than 20 lymph nodes was not associated with prolonged patient survival. For stage II disease, patient survival improved continously after lymphadenectomies of up to 40 nodes, and there was no further increase in survival thereafter. For stage III disease, a patient survival benefit was identifed when more than 50 lymph nodes were dissected. In the neoadjuvant treatment group, the lymphadenectomy extent did not influence patient survival.
Conclusion : Lymphadenectomy influenced patient survival differently depending on disease stage and neoadjuvant treatment. More extensive lymphadenectomies are necessary, especially when treating advanced disease, to improve long-term survival of patients with esophageal cancer.
책임저자: Chang Hyun Kang
Department of Thoracic and Cardiovascular Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
발표자: Samina Park, E-mail : saminapark1203@gmail.com