초록접수 현황
| 16F-017 | 구연 발표 |
The Learning Curve in Robotic Esophagectomy for Esophageal Cancer
Samina Park, MD, KwanYong Hyun, MD, Yoohwa Hwang, MD, Hyun Joo Lee, MD, PhD, In Kyu Park, MD, PhD, Young Tae Kim, MD, PhD, Chang Hyun Kang, MD, PhD
Department of Thoracic and Cardiovascular Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
Background : Robotic esophageal cancer surgery enables radical and meticulous dissection of esophagus and lymph nodes in minimally invasive way, which may reduce postoperative complications and improve oncologic outcomes. However, robotic esophagectomy is a technically demanding procedure and requires significant learning period. We aimed to identify serial surgical proficiency gain by analyzing short-term outcomes of robotic esophagectomy.
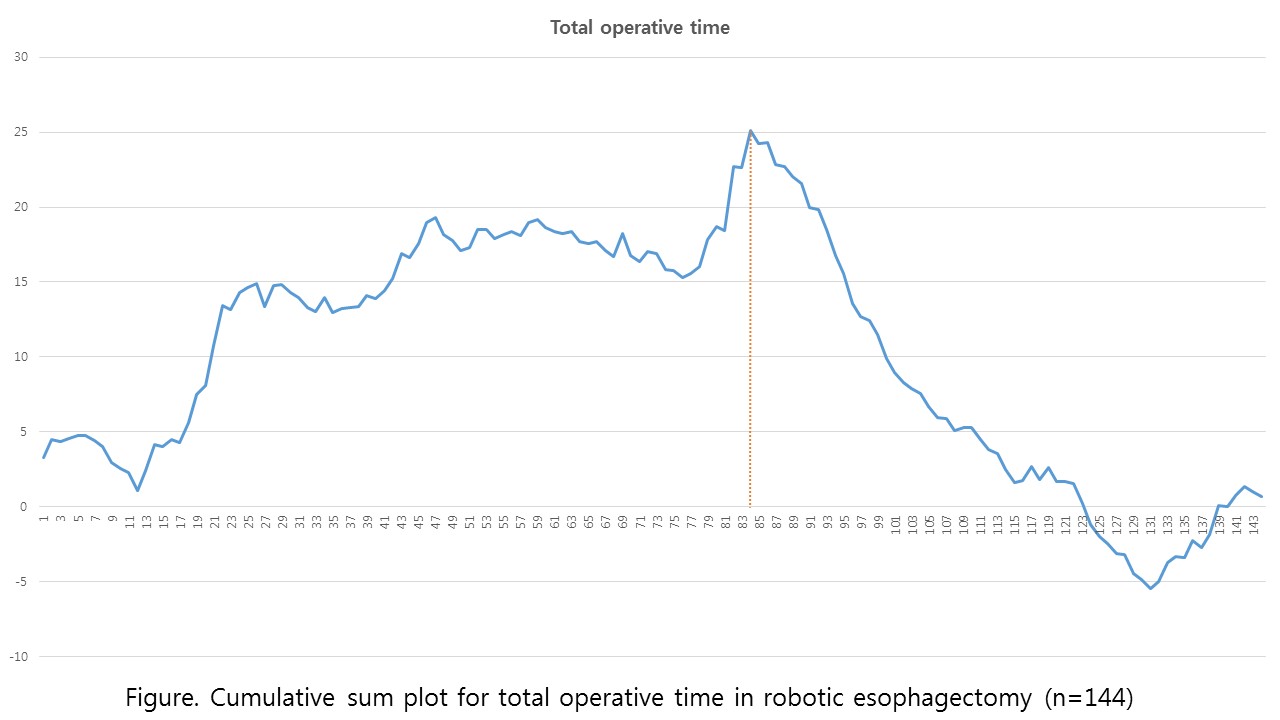
Methods : We conducted a retrospective review of patients who underwent robotic esophagectomy from May 2008 to July 2016. Early outcome measures including total operation time, thoracic procedure time, length of hospital stay, the number of harvested lymph nodes, and postoperative complications were analyzed. Cumulative sum curves were constructed to identify change-point for proficiency gain.
Results : A total of 144 patients with median age of 66 years were included. Squamous cell carcinoma (n=135, 93.8%) in upper and mid thoracic esophaguas was dominant type. Cervical anastomosis and thoracic anastomosis was performed in 111 (77%) and 33 patient (23%), respectively. Recurrent laryngeal lymph node dissection was performed in 123 patients (85%). 30-day and 90-day mortality occurred in 1 (0.7%) and 4 patients (2.7%). Two major change-points could be identified around 30th case and 80th case. After 1st change-point thoracic procedure time decreased (212 mintuets vs. 180 minutes, p=0.02), number of harvested lymph nodes increased (29 vs. 46, p<0.001), and respiratory complication rate decreased (16% vs. 6%, p=0.13). After 2nd change-point total operation time decreased (502 minutes vs. 431 minutes, p<0.001), leakage rate decreased (15% vs. 2%, p=0.008), and length of hostpital stay decreased (24 days vs. 14 days p=0.003). Vocal cord palsy rate decreased after 63rd case (35% vs. 12%, p=0.001).
Conclusion : We demonstrated temporal changes of perioperative outcomes by cumulated experience in robotic esophagectomy. Thoracic procedure related outcomes were improved in relatively early period, however overall outcome measures were improved in later period.
Methods : We conducted a retrospective review of patients who underwent robotic esophagectomy from May 2008 to July 2016. Early outcome measures including total operation time, thoracic procedure time, length of hospital stay, the number of harvested lymph nodes, and postoperative complications were analyzed. Cumulative sum curves were constructed to identify change-point for proficiency gain.
Results : A total of 144 patients with median age of 66 years were included. Squamous cell carcinoma (n=135, 93.8%) in upper and mid thoracic esophaguas was dominant type. Cervical anastomosis and thoracic anastomosis was performed in 111 (77%) and 33 patient (23%), respectively. Recurrent laryngeal lymph node dissection was performed in 123 patients (85%). 30-day and 90-day mortality occurred in 1 (0.7%) and 4 patients (2.7%). Two major change-points could be identified around 30th case and 80th case. After 1st change-point thoracic procedure time decreased (212 mintuets vs. 180 minutes, p=0.02), number of harvested lymph nodes increased (29 vs. 46, p<0.001), and respiratory complication rate decreased (16% vs. 6%, p=0.13). After 2nd change-point total operation time decreased (502 minutes vs. 431 minutes, p<0.001), leakage rate decreased (15% vs. 2%, p=0.008), and length of hostpital stay decreased (24 days vs. 14 days p=0.003). Vocal cord palsy rate decreased after 63rd case (35% vs. 12%, p=0.001).
Conclusion : We demonstrated temporal changes of perioperative outcomes by cumulated experience in robotic esophagectomy. Thoracic procedure related outcomes were improved in relatively early period, however overall outcome measures were improved in later period.
책임저자: Chang Hyun Kang
Department of Thoracic and Cardiovascular Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
발표자: Chang Hyun Kang, E-mail : chkang@snu.ac.kr