초록접수 현황
| 15F-073 | 구연 발표 |
The Oncologic Outcome of Robot-assisted Thoracoscopic Esophagectomy and the Rationale of Total Mediastinal Lymphadenectomy in Esophageal Squamous Cell Carcinoma
정희석, 남경식, 도영우, 이창영, 이진구,백효채, 정경영, 김대준
연세대학교 의과대학 세스란스병원 흉부외과학교실
Background : The oncologic outcome of robot-assisted thoracoscopic esophagectomy (RATE) for esophageal squamous cell carcinoma (ESCC) has not been reported yet worldwide. This retrospective study aims to report the oncologic outcome of RATE and to clarify the effectiveness of total mediastinal lymphadenectomy (ML) for ESCC.
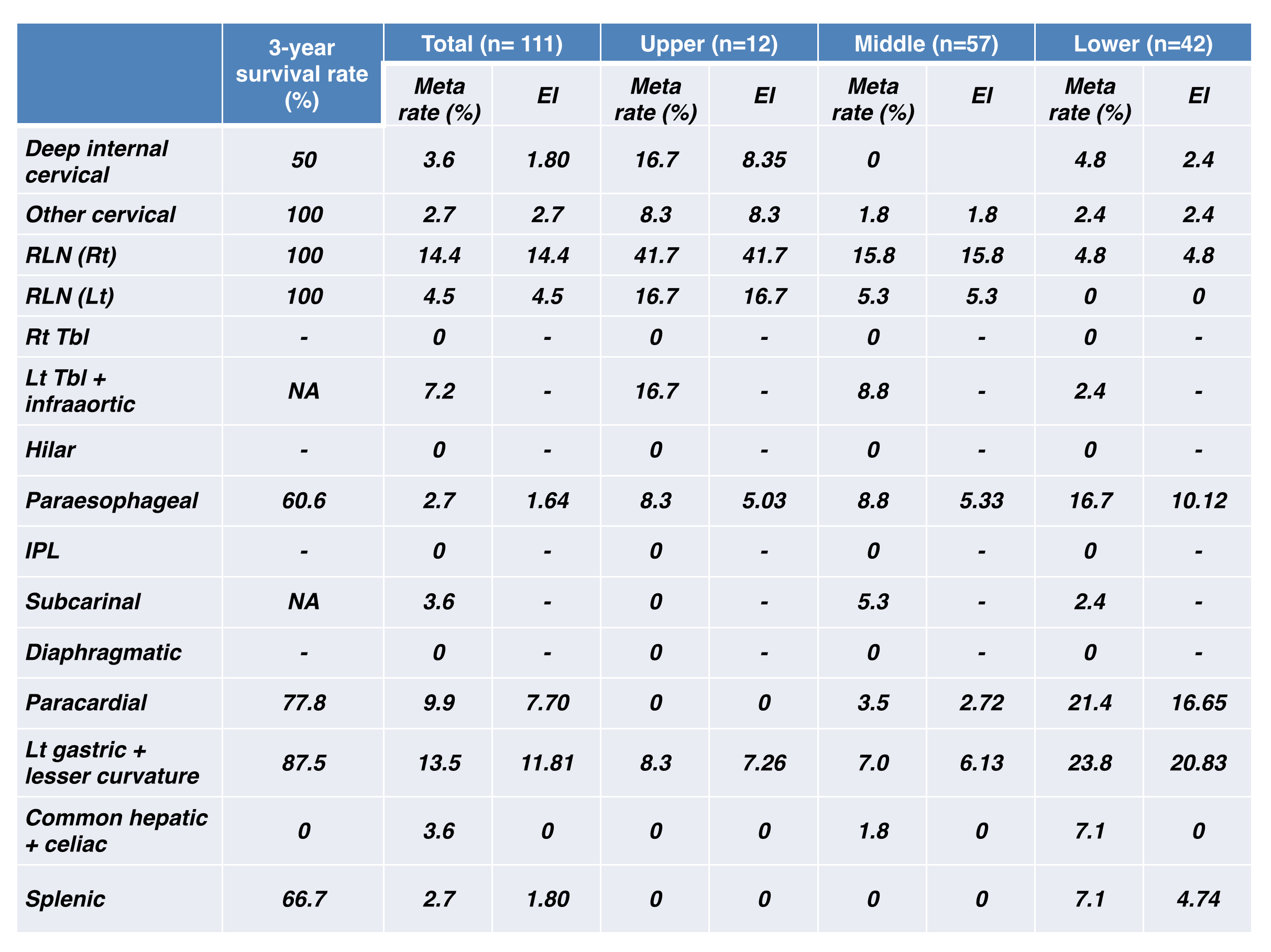
Methods : The medical records of 115 patients who underwent RATE without neoadjuvant therapy from July 2006 to December 2014 were reviewed. Efficacy index (EI) was calculated by multiplying the incidence of metastasis by the 3-year survival rate of patients for each node station, and the values of EI were compared according to main tumor location.
Results : Tumor location was upper in 12 (10.4%), middle in 59 (51.3%), and lower in 44 (38.3%). R0 resection was achieved in 110 patients (95.7%), and the number of dissected nodes was 49.0 ± 1.9. Operative mortality occurred in 4 patients (3.5%), and the mean follow-up time for 111 patients was 32.4 ± 2.2 mo. Overall survival (OS) and recur-free survival (RFS) at 3 year was 85.0% and 79.4%, respectively. The 3-year OS and RFS were 88.9% and 96.2% in stage I, 86.2% and 80.1% in stage II, and 77.8% and 79.5% in stage IIIA, respectively. Recurrent laryngeal nerve (RLN) nodes had high EI in upper and middle ESCC, and left gastric nodes had high EI in lower ESCC. Right RLN nodes showed some but limited efficacy in lower ESCC.
Conclusion : Our study demonstrated that RATE showed comparable oncologic outcome. Total ML including dissection of RLN nodes should be carried out especially in upper or middle ESCC.
Methods : The medical records of 115 patients who underwent RATE without neoadjuvant therapy from July 2006 to December 2014 were reviewed. Efficacy index (EI) was calculated by multiplying the incidence of metastasis by the 3-year survival rate of patients for each node station, and the values of EI were compared according to main tumor location.
Results : Tumor location was upper in 12 (10.4%), middle in 59 (51.3%), and lower in 44 (38.3%). R0 resection was achieved in 110 patients (95.7%), and the number of dissected nodes was 49.0 ± 1.9. Operative mortality occurred in 4 patients (3.5%), and the mean follow-up time for 111 patients was 32.4 ± 2.2 mo. Overall survival (OS) and recur-free survival (RFS) at 3 year was 85.0% and 79.4%, respectively. The 3-year OS and RFS were 88.9% and 96.2% in stage I, 86.2% and 80.1% in stage II, and 77.8% and 79.5% in stage IIIA, respectively. Recurrent laryngeal nerve (RLN) nodes had high EI in upper and middle ESCC, and left gastric nodes had high EI in lower ESCC. Right RLN nodes showed some but limited efficacy in lower ESCC.
Conclusion : Our study demonstrated that RATE showed comparable oncologic outcome. Total ML including dissection of RLN nodes should be carried out especially in upper or middle ESCC.
책임저자: 김대준
연세대학교 의과대학 세스란스병원 흉부외과학교실
연락처 : 정희석, Tel: 02-2228-2140 , E-mail : haobbang80@gmail.com