초록접수 현황
| 14F-053 | 구연 발표 |
The Role of Intra-operative Frozen Pathology with Embedding Medium Inflation Technique for the Optimal Guidance of Surgical Methods for Pulmonary Ground Glass Nodules
황유화¹, 박샘이나¹, 최진호¹, 복진산¹, 성용원², 이현주¹, 박인규¹, 강창현¹, 정두현³, 구진모⁴, 김영태¹
서울대학교 의과대학 서울대학교병원 흉부외과학교실¹, 서울특별시보라매병원 흉부외과², 서울대학교 의과대학 병리학교실³, 서울대학교 의과대학 영상의학과⁴
Background : Increasing number of lung cancer screening program frequently detects pulmonary ground glass nodules (GGN), which often require surgical resection. However, the guideline how to decide optimal surgical resection method is not well established. We applied intra-operative frozen section diagnosis using embedding medium inflation technique (EMIT) and compared its usefulness to that of convention method in terms of guiding an optimal surgical resection.
Methods : We prospectively set up 41 GGN patients and applied EMIP method. For comparison, 154consecutive GGN cases where the conventional frozen diagnosis was used were set. The diagnostic accuracy as well as its role to guide optimal surgical methods was compared between two groups with a gold standard being that of final pathologic diagnosis. Optimal surgical method was defined as wedge resection if the final pathologies were benign, AAH, adenocarcinoma in situ (AIS) or microinvasive adenocarcinoma (MIA) and as anatomic resection (lobectomy or segmentectomy) if the lesions were invasive adenocarcinoma.
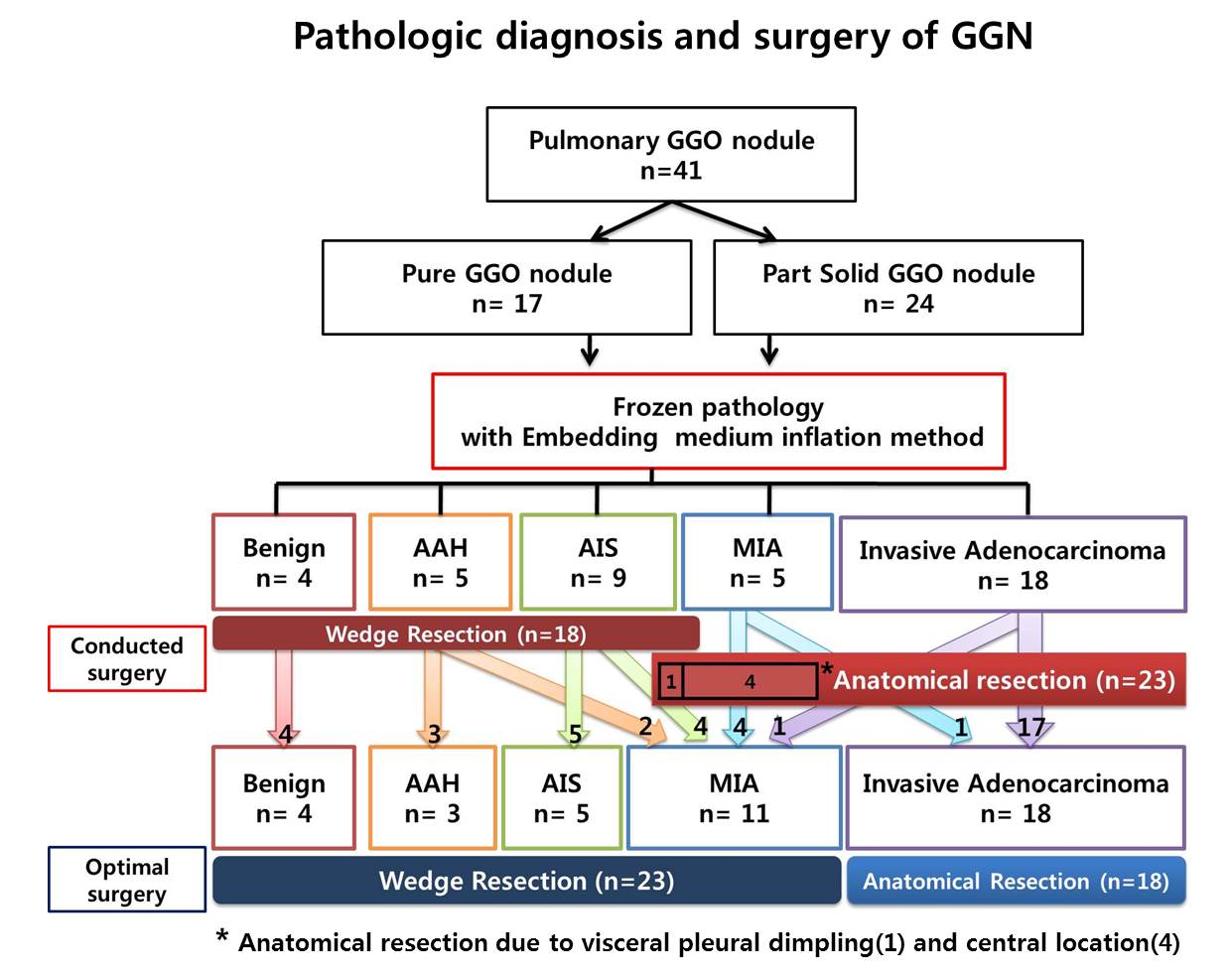
Results : There were no differences in nodule sizes between the conventional group and EMIT group (1.45±0.6 versus 1.51±0.5, p=0.63). In conventional group, 138 nodules were correctly classified as to either malignant or benign lesion (sensitivity 95.6%, specificity 53.8%). Anatomic resections should have been applied in 5 patients. Actually, one patient underwent a second round of anatomic operation. In EMIT group, 38of 41nodules were correctly classified (sensitivity 100%, specificity 66.7%). In five patients, anatomic resections were performed despite the diagnosis of MIA or AIS: in one, because gross finding suggested visceral pleural dimpling, in four, because the lesions were centrally located. In one patient among those four, the diagnosis changed from MIA to invasive adenocarcinoma. However as the invasive portion was only 7mm, he did not require second operation. As a consequence, none of patient received inadequate, non-anatomic resection because of erroneous frozen diagnosis in EMIT group. (Figure)
Conclusion : The diagnostic accuracy of EMIT in GGO nodules was superior to that of conventional method. Furthermore, EMIT could accurately guide surgeons to decide optimal surgical resection by providing accurate size estimation of the invasive components of the GGN intraoperatively.
Methods : We prospectively set up 41 GGN patients and applied EMIP method. For comparison, 154consecutive GGN cases where the conventional frozen diagnosis was used were set. The diagnostic accuracy as well as its role to guide optimal surgical methods was compared between two groups with a gold standard being that of final pathologic diagnosis. Optimal surgical method was defined as wedge resection if the final pathologies were benign, AAH, adenocarcinoma in situ (AIS) or microinvasive adenocarcinoma (MIA) and as anatomic resection (lobectomy or segmentectomy) if the lesions were invasive adenocarcinoma.
Results : There were no differences in nodule sizes between the conventional group and EMIT group (1.45±0.6 versus 1.51±0.5, p=0.63). In conventional group, 138 nodules were correctly classified as to either malignant or benign lesion (sensitivity 95.6%, specificity 53.8%). Anatomic resections should have been applied in 5 patients. Actually, one patient underwent a second round of anatomic operation. In EMIT group, 38of 41nodules were correctly classified (sensitivity 100%, specificity 66.7%). In five patients, anatomic resections were performed despite the diagnosis of MIA or AIS: in one, because gross finding suggested visceral pleural dimpling, in four, because the lesions were centrally located. In one patient among those four, the diagnosis changed from MIA to invasive adenocarcinoma. However as the invasive portion was only 7mm, he did not require second operation. As a consequence, none of patient received inadequate, non-anatomic resection because of erroneous frozen diagnosis in EMIT group. (Figure)
Conclusion : The diagnostic accuracy of EMIT in GGO nodules was superior to that of conventional method. Furthermore, EMIT could accurately guide surgeons to decide optimal surgical resection by providing accurate size estimation of the invasive components of the GGN intraoperatively.
책임저자: 김영태
서울대학교 의과대학 서울대학교병원 흉부외과학교실
연락처 : 황유화, Tel: 02-2072-7212 , E-mail : syooflower@gmail.com