초록접수 현황
| 14F-261 | 구연 발표 |
The Outcome of Primary Repair of the Transposition of the Great Arteries or Variants and Aortic Arch Obstruction.
방지현, 박정준, 윤태진, 박천수
Division of Pediatric Cardiac Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
Background : The transposition of the great arteries (TGA) or variants associated with arch obstruction presents a surgical challenge. The standard surgical option for this combination is primary repair with arterial switch operation (ASO) and arch reconstruction. We investigated the outcomes especially focusing on reoperation or reintervention after anatomical repair for these patients during recent 10 years.
Methods : Between January 2004 and July 2014, 27 patients with TGA(n=11) or Taussig-Bing anomaly (n=16) with arch obstruction underwent an anatomoical repair with ASO and arch reconstruction. Age and weight at operation were 17 days (range, 4 - 180 days) and 3.33kg (range, 2.6 - 5.3 kg), respectively. The aortic arch was reconstructed with native tissues in 23 patients, using autologous main pulmonary arterial patch in 4 patients (14%). Right ventricular outflow tract (RVOT) was augmented with resection or division of the conus in 4 patients (4/27, 14%) and using a patch in one patient (1/27, 3.7%). Cardiopulmonary bypass time and ischemic time were 260 minutes (range, 154 - 4317 minutes) and 140 minutes (range, 102 – 303 minutes), respectively.
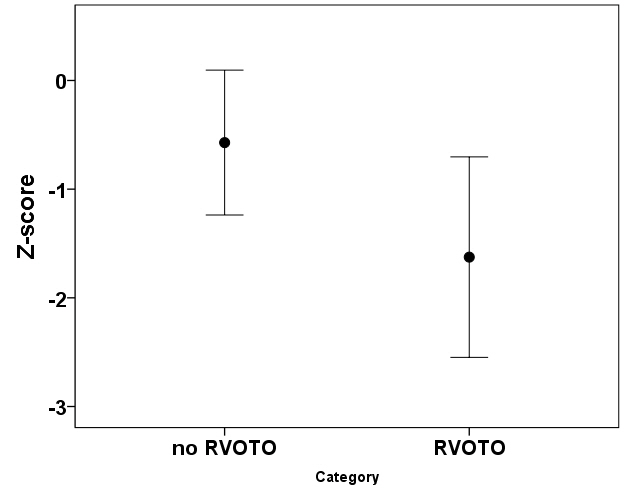
Results : There were 4 in-hospital deaths (4/27, 14.8%) and 2 late deaths at 6 months and 65 months after the operation, respectively. In univariate analysis, risk factors for mortality were intraoperative coronary revision (p<0.001), postoperative right ventricular outflow obstruction (RVOTO) (p<0.02) and longer cardiopulmonary bypass time (p<0.001). Follow-up duration was 46 months. Significant RVOTO was present in 7 patients. Two of them was died in hospital and 6months after the operation. There have been been 7 reoperations or reinterventions in 5 patients for RVOTO (5/23, 21.7%) during follow-up. There was no reoperation or reintervention for arch obstruction. Patients with significant RVOTO semms to have small preoperative aortic valve z-score (-0.57±1.4 vs. -1.6±1.0, p=0.130) (Figure 1) and might be related with interrupted aortic arch (4/8 vs. 3/19, p=0.145).
Conclusion : Early outcome after primary repair of TGA or variant and arch obstruction seems to be acceptable. However, late RVOTO is a major concern and might be associated with severity of the arch obstruction and the size of the aortic valve in preoperative evaluation.
Methods : Between January 2004 and July 2014, 27 patients with TGA(n=11) or Taussig-Bing anomaly (n=16) with arch obstruction underwent an anatomoical repair with ASO and arch reconstruction. Age and weight at operation were 17 days (range, 4 - 180 days) and 3.33kg (range, 2.6 - 5.3 kg), respectively. The aortic arch was reconstructed with native tissues in 23 patients, using autologous main pulmonary arterial patch in 4 patients (14%). Right ventricular outflow tract (RVOT) was augmented with resection or division of the conus in 4 patients (4/27, 14%) and using a patch in one patient (1/27, 3.7%). Cardiopulmonary bypass time and ischemic time were 260 minutes (range, 154 - 4317 minutes) and 140 minutes (range, 102 – 303 minutes), respectively.
Results : There were 4 in-hospital deaths (4/27, 14.8%) and 2 late deaths at 6 months and 65 months after the operation, respectively. In univariate analysis, risk factors for mortality were intraoperative coronary revision (p<0.001), postoperative right ventricular outflow obstruction (RVOTO) (p<0.02) and longer cardiopulmonary bypass time (p<0.001). Follow-up duration was 46 months. Significant RVOTO was present in 7 patients. Two of them was died in hospital and 6months after the operation. There have been been 7 reoperations or reinterventions in 5 patients for RVOTO (5/23, 21.7%) during follow-up. There was no reoperation or reintervention for arch obstruction. Patients with significant RVOTO semms to have small preoperative aortic valve z-score (-0.57±1.4 vs. -1.6±1.0, p=0.130) (Figure 1) and might be related with interrupted aortic arch (4/8 vs. 3/19, p=0.145).
Conclusion : Early outcome after primary repair of TGA or variant and arch obstruction seems to be acceptable. However, late RVOTO is a major concern and might be associated with severity of the arch obstruction and the size of the aortic valve in preoperative evaluation.
책임저자: 박천수
울산대학교 의과대학 서울아산병원 흉부외과학교실
연락처 : 방지현, Tel: 02-3010-1853 , E-mail : mibbi@naver.com