초록접수 현황
| 14F-213 | 포스터 발표 |
Total Occlusion of Trachea due to Primary Tracheal Squamous Cell Carcinoma with Respiratory Arrest : Mass Excision with Veno-veno ECMO (Extracorporeal Membrane Oxygenation)
이연주, 한성준, 정유영, 강신광, 나명훈, 유재현, 임승평, 강민웅
Department of Thoracic and Cardiovascular Surgery, School of Medicine, Chungnam National University, Daejeon, Republic of Korea
Background : Primary tracheal tumors are rare, composing only 0.2% of thoracic cancers. Of all primary tracheal tumors, 80% are malignant. Regardless of the histology type, however, tracheal tumors patients can present with catastrophic airway obstruction that can cause fatal complications. Therefore, prompt action and appropriate treatment is important for positive outcome. We report a case in which ECMO effectively substituted the lungs during emergent tracheal tumor resection with respiratory arrest.
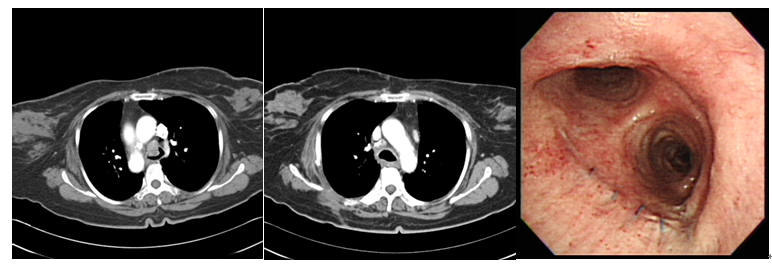
Methods : A 68-year-old female patient visited the emergency ward after suffering from sudden onset dyspnea and coughing for three days. Chest CT revealed that large mass within 1cm proximal to the carina was almost completely obstructing the endotracheal lumen. After admission, cardiac arrest was occurred and we immediately preformed extracorporeal cardioplulmonary resuscitation with veno-veno ECMO and emergency operation.
The pleural cavity was approached via 5th ICS from posterolateral thoracotomy. The location of tumor was identified using bronchoscopic light and made incision on trachea. We utilised bronchial blocker to obstruct both main bronchus to prevent tumor disseminate and then excised the tumor with trachea. The tracheal was anastomosed with 4-0 prolene interrupted suture.
Results : ECMO was weaned 3 days post-operation, and endotracheal tube extubated 5 days after the operation. As histologic type was squamous cell carcinoma. There was no recurrence for the 28 months follow up period.
Conclusion : ECMO can serve a critical role in both responding to respiratory failure and facilitating tranchea tumor resection when possibly fatal obstruction of the endotranchea lumen is present.
Methods : A 68-year-old female patient visited the emergency ward after suffering from sudden onset dyspnea and coughing for three days. Chest CT revealed that large mass within 1cm proximal to the carina was almost completely obstructing the endotracheal lumen. After admission, cardiac arrest was occurred and we immediately preformed extracorporeal cardioplulmonary resuscitation with veno-veno ECMO and emergency operation.
The pleural cavity was approached via 5th ICS from posterolateral thoracotomy. The location of tumor was identified using bronchoscopic light and made incision on trachea. We utilised bronchial blocker to obstruct both main bronchus to prevent tumor disseminate and then excised the tumor with trachea. The tracheal was anastomosed with 4-0 prolene interrupted suture.
Results : ECMO was weaned 3 days post-operation, and endotracheal tube extubated 5 days after the operation. As histologic type was squamous cell carcinoma. There was no recurrence for the 28 months follow up period.
Conclusion : ECMO can serve a critical role in both responding to respiratory failure and facilitating tranchea tumor resection when possibly fatal obstruction of the endotranchea lumen is present.
책임저자: 강민웅
Department of Thoracic and Cardiovascular Surgery, School of Medicine, Chungnam National University, Daejeon, Republic of Korea
연락처 : 이연주, Tel: 042-280-7374 , E-mail : yooychong@gmail.com