초록접수 현황
| 14F-001 | 포스터 발표 |
Reinforcement with Pericardial Flap after Delayed Closure of an Esophageal Fistula for Patient with Boerhaave Syndrome
김수완, 이석재, 장지원
제주대학교 의학전문대학원 흉부외과학교실
Background : Boerhaave syndrome is a serious condition with significantly high morbidity and mortality rates despite advances in diagnostics, surgery, and critical care. The most important factor that affects prognosis is surgery, with an optimal time being within 24 hours. The incidence of leakage resulting from severe inflammation following an esophageal repair sharply increases 24 hours after the esophageal perforation, and most patients die of mediastinitis and sepsis.
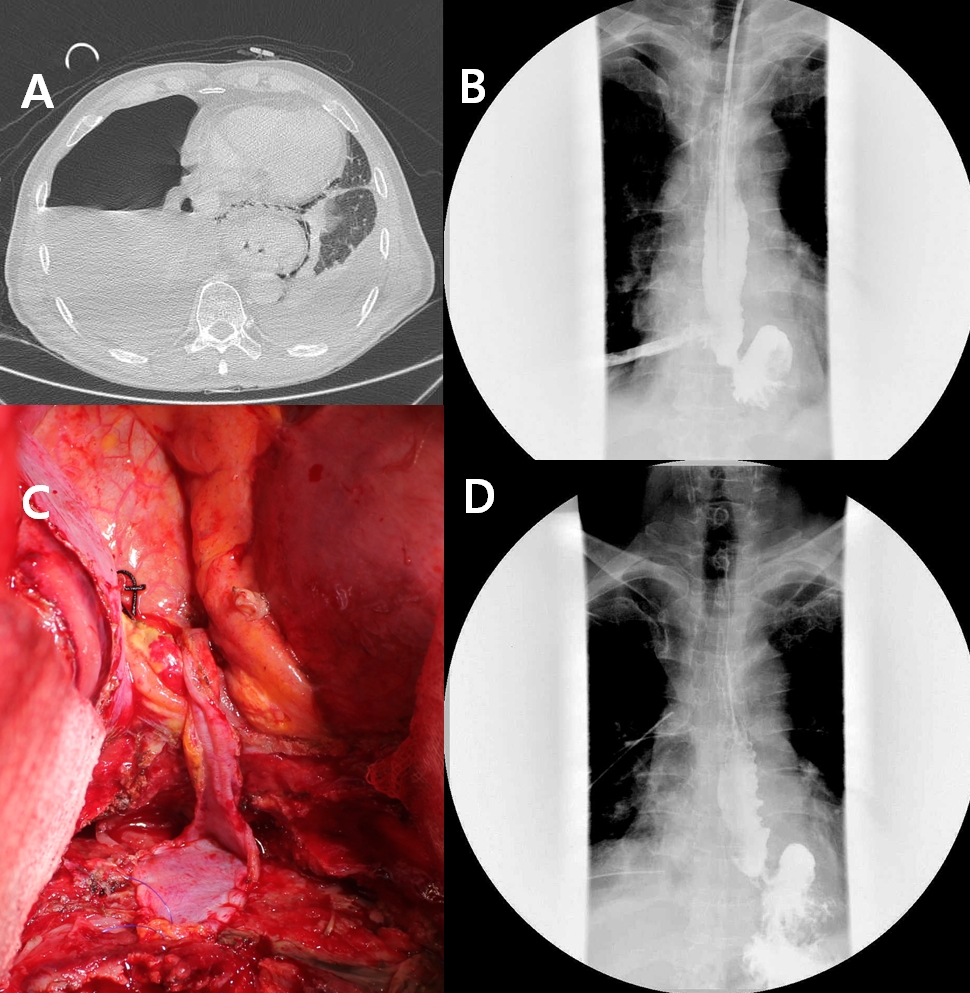
Methods : A 59-year-old male patient was transferred from a local hospital 48 hours following a delayed diagnosis of esophageal perforation. The patient suffered from abrupt dyspnea and chest pain after vomiting. An initial computerized tomography showed a massive right pneumothorax and bilateral pleural effusions (A). Distal esophageal perforation was confirmed by esophagogram. The gastrograffin-contrast was passed through the chest tube (B). The patient was supported by mechanical ventilation for stuporous mentality and septic shock. The patient was conservatively managed with a chest tube drainage of an empyema, using broad-spectrum antibiotics, total parenteral nutrition, and hydration. A right thoracotomy was performed 18 days after the esophageal perforation. We could not point out the perforated site because of dense adhesions of the parietal and mediastinal pleura. We identified a fistula tract between the esophagus and the thickened mediastinum, and closed the fistula opening with several interrupted Black-silk sutures. We reinforced the obliterated fistula using a continuous running suture with polyprophylene and the autologous pericardium which had been harvested longitudinally following the phrenic nerve (C). The outer surface of the pericardium containing the rich fat tissues faced the fistula. The pericardial defect, after the harvesting, was closed by interrupted sutures with black-silk.
Results : There was no esophageal leakage (D), and the patient could tolerate a soft diet orally 10 days after the operation. He was discharged 49 days postoperatively, and followed-up for 2 months after increasing to a normal diet.
Conclusion : A general strategy of surgical repair for esophageal perforation is the separated primary closure of the esophageal mucosa and the muscle layers. We successfully repaired the esophagus by fistula closure and reinforcement with a pericardial flap, even if we could not perform a primary closure of the esophagus.
Methods : A 59-year-old male patient was transferred from a local hospital 48 hours following a delayed diagnosis of esophageal perforation. The patient suffered from abrupt dyspnea and chest pain after vomiting. An initial computerized tomography showed a massive right pneumothorax and bilateral pleural effusions (A). Distal esophageal perforation was confirmed by esophagogram. The gastrograffin-contrast was passed through the chest tube (B). The patient was supported by mechanical ventilation for stuporous mentality and septic shock. The patient was conservatively managed with a chest tube drainage of an empyema, using broad-spectrum antibiotics, total parenteral nutrition, and hydration. A right thoracotomy was performed 18 days after the esophageal perforation. We could not point out the perforated site because of dense adhesions of the parietal and mediastinal pleura. We identified a fistula tract between the esophagus and the thickened mediastinum, and closed the fistula opening with several interrupted Black-silk sutures. We reinforced the obliterated fistula using a continuous running suture with polyprophylene and the autologous pericardium which had been harvested longitudinally following the phrenic nerve (C). The outer surface of the pericardium containing the rich fat tissues faced the fistula. The pericardial defect, after the harvesting, was closed by interrupted sutures with black-silk.
Results : There was no esophageal leakage (D), and the patient could tolerate a soft diet orally 10 days after the operation. He was discharged 49 days postoperatively, and followed-up for 2 months after increasing to a normal diet.
Conclusion : A general strategy of surgical repair for esophageal perforation is the separated primary closure of the esophageal mucosa and the muscle layers. We successfully repaired the esophagus by fistula closure and reinforcement with a pericardial flap, even if we could not perform a primary closure of the esophagus.
책임저자: 이석재
제주대학교 의학전문대학원 흉부외과학교실
연락처 : 김수완, Tel: 064-717-1704 , E-mail : 95swan@gmail.com